Editor’s Note: The Atlantic is making vital coverage of the coronavirus available to all readers. Find the collection here.
Edward Lorenz was just out of college when he was recruited into World War II. He was assigned to be a weather forecaster, despite having no experience in meteorology. What Lorenz knew was math.
So he started experimenting with differential equations, trying to make predictions based on patterns in data on past temperatures and pressures. One day, while testing his system, he repeated a simulation with a few decimals rounded off in the data. To his surprise, a radically different future emerged.
He called this finding “the butterfly effect.” In a complex model, where each day’s weather influences the next day’s, a tweak in initial conditions can have wild downstream consequences. The butterfly effect became central to the emerging field of chaos theory, which has since been applied to economics, sociology, and many other subjects, in attempts to deconstruct complex phenomena. That field is now helping predict the future of the pandemic—in particular, how it ends.
[Read: How the pandemic will end]
Chaos theory applies neatly to the spread of the coronavirus, in that seemingly tiny decisions or differences in reaction speed can have inordinate consequences. Effects can seem random when, in fact, they trace to discrete decisions made long prior. For example, the United States has surpassed 125,000 deaths from COVID-19. Having suppressed the virus early, South Korea has had only 289. Vietnam’s toll sits at zero. Even when differences from place to place appear random, or too dramatic to pin entirely on a failed national response, they are not.
There is enormous variation even within the U.S., which could also seem chaotic. Some places took limited measures and were barely hit; others locked down but suffered greatly. New York City has been slowly reopening since early June, but despite that—and despite mass outdoor gatherings in the throes of civil unrest over the past six weeks—the city has not seen even a small increase in daily reported cases. By contrast, other cities that have attempted to reopen have seen incapacitating surges.
But just as barely predictable meteorological events arise from totally predictable laws of physics, the complex dynamics of a pandemic center on an extremely limited set of concepts in basic viral biology. Early failures to test and shut down in the U.S. have been amplified through the butterfly effect. Current decisions will be as well.
When phenomena appear chaotic, mathematical modelers make it their job to find the underlying order. Once models can accurately describe the real world, as some now do, they gain the predictive power to give clearer glimpses into likely futures.
In mid-February, the Harvard epidemiologist Marc Lipsitch told me that this virus could infect most people in the United States if the country’s leaders did not take action. At the time, the U.S. had only a handful of confirmed cases. Few people were imagining the future Lipsitch saw—in which millions, even hundreds of millions, of Americans could fall ill. This was, at least in part, because we weren’t testing for the virus.
[Read: You’re likely to get the coronavirus]
Lipsitch even received some criticism from scientists who felt uncomfortable with his estimate, since there were so little data to go on. Indeed, at that point, many futures were still possible. But when a virus spreads as quickly and effectively as this one was spreading in February—killing many while leaving others who had few or no symptoms to spread the disease—that virus can be expected to run its course through a population that does not take dramatic measures.
Now, based on the U.S. response since February, Lipsitch believes that we’re still likely to see the virus spread to the point of becoming endemic. That would mean it is with us indefinitely, and the current pandemic would end when we reach levels of “herd immunity,” traditionally defined as the threshold at which enough people in a group have immune protection so the virus can no longer cause huge spikes in disease.
The concept of herd immunity comes from vaccination policy, in which it’s used to calculate the number of people who need to be vaccinated in order to ensure the safety of the population. But a coronavirus vaccine is still far off, and last month, Anthony Fauci, the head of the National Institute of Allergy and Infectious Diseases, said that, because of a “general anti-science, anti-authority, anti-vaccine feeling,” the U.S. is “unlikely” to achieve herd immunity even after a vaccine is available.
Back in February, Lipsitch gave a very rough estimate that, absent intervention, herd immunity might happen after 40 to 70 percent of the population had been infected. The idea of hitting this level of infection implied grim forecasts about disease and death. The case-fatality rate for COVID-19 is now very roughly 1 percent overall. In the absolute simplest, linear model, if 70 percent of the world were to get infected, that would mean more than 54 million deaths.
But the effects of the coronavirus are not linear. The virus affects individuals and populations in very different ways. The case-fatality rate varies drastically between adults under 40 and the elderly. This same characteristic variability of the virus—what makes it so dangerous in early stages of outbreaks—also gives a clue as to why those outbreaks could burn out earlier than initially expected. In countries with uncontained spread of the virus, such as the U.S., exactly what the herd-immunity threshold turns out to be could make a dramatic difference in how many people fall ill and die. Without a better plan, this threshold—the percentage of people who have been infected that would constitute herd immunity—seems to have become central to our fates.
Some mathematicians believe that it’s much lower than initially imagined. At least, it could be, if we choose the right future.
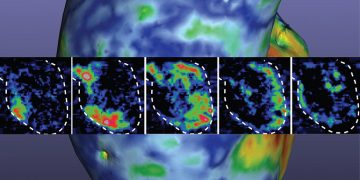
Gabriela Gomes studies chaos. Specifically, patterns in nonlinear dynamics. She was drawn to the field by something called frailty variation—why the same diseases manifest so differently from one person to the next. She uses mathematics to deconstruct the chains of events that can lead two people with the same disease to have wildly different outcomes.
So with all its apparently chaotic eccentricities, the coronavirus was an ideal challenge for Gomes, a professor at the University of Strathclyde, in Glasgow, Scotland. For the past few months, she has been collaborating with an international group of mathematicians to run models that incorporate the many variations in how this virus seems to be affecting people. Her goal has been to move as far away from simple averages as possible, and to incorporate as many of the disparate effects of the virus as possible when making new forecasts.
In normal times, herd immunity is calculated based on a standardized intervention with predictable results: vaccination. Everyone is exposed to the same (or very similar) immune-generating viral components. We are able to calculate what percentage of people need that exposure in order to develop meaningful immunity across the population.
This is not the case when a virus is spreading in the real world. Instead, the complexities of real life create what modelers refer to as heterogeneity. People are exposed to different amounts of the virus, in different contexts, via different routes. A virus that is new to the species creates more variety in immune responses. Some of us are more susceptible to being infected, and some are more likely to transmit the virus once infected. Even small differences in individual susceptibility and transmission can, as with any chaos phenomenon, lead to very different outcomes as the effects compound over time, on the scale of a pandemic. As Gomes explains, “There doesn’t need to be a lot of variation in a population for epidemics to slow down quite drastically.”
[Read: A devastating new stage of the pandemic]
In a pandemic, the heterogeneity of the infectious process also makes forecasting difficult. When you flip a coin, the outcome is not affected by the flips prior. But in dynamic systems, the outcomes are more like those in chess: The next play is influenced by the previous one. Differences in outcome can grow exponentially, reinforcing one another until the situation becomes, through a series of individually predictable moves, radically different from other possible scenarios. You have some chance of being able to predict the first move in a game of chess, but good luck predicting the last.
That’s exactly what Gomes’s work attempts to do. She describes a model in which everyone is equally susceptible to coronavirus infection (a homogeneous model), and a model in which some people are more susceptible than others (a heterogeneous model). Even if the two populations start out with the same average susceptibility to infection, you don’t get the same epidemics. “The outbreaks look similar at the beginning. But in the heterogeneous population, individuals are not infected at random,” she told me. “The highly susceptible people are more likely to get infected first. As a result, the average susceptibility gets lower and lower over time.”
Effects like this—“selective depletion” of people who are more susceptible—can quickly decelerate a virus’s spread. When Gomes uses this sort of pattern to model the coronavirus’s spread, the compounding effects of heterogeneity seem to show that the onslaught of cases and deaths seen in initial spikes around the world are unlikely to happen a second time. Based on data from several countries in Europe, she said, her results show a herd-immunity threshold much lower than that of other models.
“We just keep running the models, and it keeps coming back at less than 20 percent,” Gomes said. “It’s very striking.”
If that proves correct, it would be life-altering news. It wouldn’t mean that the virus is gone. But by Gomes’s estimates, if roughly one out of every five people in a given population is immune to the virus, that seems to be enough to slow its spread to a level where each infectious person is infecting an average of less than one other person. The number of infections would steadily decline. That’s the classic definition of herd immunity. It would mean, for instance, that at 25 percent antibody prevalence, New York City could continue its careful reopening without fear of another major surge in cases.
[Read: A guide to staying safe as states reopen]
It doesn’t make intuitive sense, Gomes admits, but “the homogenous models just don’t make curves that match the current data,” she said. Dynamic systems develop in complex and unpredictable ways, and she believes that the best we can do is continually update models based on what is happening in the real world. She can’t say why the threshold in her models is consistently at or below 20 percent, but it is. “If heterogeneity isn’t the cause,” she said, “then I’d like for someone to explain what is.”
At Stockholm University, Tom Britton, the dean of mathematics and physics, thinks that a 20 percent threshold is unlikely, but not impossible. His lab has also been building epidemiological models based on data from around the globe. He believes that variation in susceptibility and exposure to the virus clearly seems to be reducing estimates for herd immunity. Britton and his colleagues recently published their model, demonstrating the effect, in Science.
“If there is a large variability of susceptibility among humans, then herd immunity could be as low as 20 percent,” Britton told me. But there’s reason to suspect that people do not have such dramatically disparate susceptibility to the coronavirus. High degrees of variability are more common in things such as sexually transmitted infections, where a person with 100 partners a year is far more susceptible than someone celibate. Respiratory viruses tend to be more equal-opportunity invaders. “I don’t think it will happen at 20 percent,” Britton said. “Between 35 and 45 percent—I think that would be a level where spreading drops drastically.”
Models like Britton’s and Gomes’s also assume that, after infection, people obtain immunity. This is a clear caveat that all the researchers make. COVID-19 is a new disease, so no one can be sure that infected people become immune reliably, or how long immunity lasts. But Britton noted that there are no clear instances of double infections so far, which suggests that this virus creates immunity for at least some meaningful length of time, as most viruses do.
Lipsitch also believes that heterogeneity is important to factor into any model. It was one reason he updated his prediction, not long after we spoke in February, of what the herd-immunity threshold would be. Instead of 40 to 70 percent, he lowered it to 20 to 60 percent. When we spoke last week, he said he still stands by that, but he is skeptical that the number lands close to the 20 percent end of the range. “I think it’s unlikely,” he said, but added, “This virus is proving there can be orders-of-magnitude differences in attack rates, depending on political and societal decisions, which I don’t know how to forecast.”
“I think we all agree that heterogeneity is important,” says Kate Langwig, a professor at Virginia Tech. She studied at Harvard under Lipsitch, and was also mentored by Gomes. Biological variations in susceptibility could come down to factors as simple as who has more nose hair, or who talks the loudest and most explosively, and Langwig shares the belief that these factors can create heterogeneity in susceptibility and transmission. Those effects can compound to dramatically change the math behind predictions for the future.
But she declines to endorse any particular numeric threshold for herd immunity. She’s not comfortable with the idea of a single number at all. What’s important to her, rather, is that people are not misled by the idea of herd immunity. In the context of vaccination, herd-immunity thresholds are relatively fixed and predictable. In the context of an ongoing pandemic, thinking of this threshold as some static concept can be dangerously misleading.
[Read: The U.K.’s coronavirus ‘herd immunity’ debacle]
“During the last few months, we’ve started talking about ‘natural herd immunity’ and what would be used to block future waves,” says Shweta Bansal, an associate professor at Georgetown University who studies how social interactions influence infectious diseases. She worries that many people conflate academic projections about reaching herd immunity with a “let it run wild” fatalism. “My view is that trying to take that route would lead to mass death and devastation,” she says.
Indeed, letting a new, rapidly spreading virus run unchecked in a population with zero immunity could mean that nearly everyone in a given location gets infected. With vaccination, the herd-immunity threshold is vital to guiding policy and medical practice: If about 90 percent of people are vaccinated against measles, for example, then, accounting for waning antibodies and variable immune responses, it’s safe to assume that 60 or 70 percent are protected and the population isn’t at risk of an outbreak. But that concept doesn’t clearly apply when a highly contagious virus hits a population with zero immunity. Left totally unchecked, Bansal says, the percentage of infected people could go even higher than 70 percent.
By definition, dynamic systems don’t deal in static numbers. Any such herd-immunity threshold is context-dependent and constantly shifting. It will change over time and space. It varies depending on the basic reproduction number—the average number of new infections caused by an infected individual. During the early stage of an outbreak of a new virus (to which no one has immunity), that number will be higher. The number is skewed by super-spreading events, such as when one person in a choir infects 50 others. And the number in a dense city such as New York should be expected to be higher than that in rural Alaska. “Within certain populations that lack heterogeneity, like within a nursing home or school, you may even see the herd-immunity threshold be above 70 percent,” Bansal says. If a population average led people in those settings to get complacent, there could be needless death.
[Read: The U.S. is repeating its deadliest pandemic mistake]
For all the mysteries of how this virus affects our bodies and immune systems, and all the heterogeneity involved in the complex modeling of outcomes, Bansal believes that heterogeneity of behavior is the key determinant of our futures. “That magic number that we’re describing as a herd-immunity threshold very much depends on how individuals behave,” Bansal says, since R0 clearly changes with behaviors. On average, the R0 of the coronavirus currently seems to be between 2 and 3, according to Lipsitch. But if we all sealed ourselves in isolation pods today, the R0 would drop to zero. There would be no more deaths.
“COVID-19 is the first disease in modern times where the whole world has changed their behavior and disease spread has been reduced,” Britton noted. That made old models and numbers obsolete. Social distancing and other reactive measures changed the R0 value, and they will continue to do so. The virus has certain immutable properties, but there is nothing immutable about how many infections it causes in the real world.
What we seem to need is a better understanding of herd immunity in this novel context. The threshold can change based on how a virus spreads. The spread keeps on changing based on how we react to it at every stage, and the effects compound. Small preventive measures have big downstream effects. In other words, the herd in question determines its immunity. There is no mystery in how to drop the R0 to below 1 and reach an effective herd immunity: masks, social distancing, hand-washing, and everything everyone is tired of hearing about. It is already being done.
Essentially, at present, New York City—where I live—might be said to be at a version of herd immunity, or at least safe equilibrium. Our case counts are very low. They have been low for weeks. Our antibody counts mean that a not-insignificant number of people are effectively removed from the chain of transmission. Many more can be effectively excluded because they’re staying isolated and distanced, wearing masks, and being hygienically vigilant. If we keep living just as we are, another big wave of disease seems unlikely.
[Read: Don’t close parks. Open up the streets.]
Lipsitch stands by the February projection that Americans are likely to get the coronavirus, but not because that’s the only possible future. In other countries, it isn’t the case. “I think it no longer seems impossible that Switzerland or Germany could remain near where they are in terms of cases, meaning not very much larger outbreaks, until there’s a vaccine,” he said. They seem to have the will and systems in place to keep their economies closed enough to maintain their current equilibrium.
Other wealthy countries could hypothetically create societies that are effectively immune to further surges, where the effective herd-immunity threshold is low. Even in the U.S., it’s not too late to create a world in which you are not likely to get the coronavirus. We can wear masks and enable people to stay housed and fed without taking up dangerous work. But, judging by the decisions U.S. leaders have made so far, it seems that few places in the country will choose to live this way. Many cities and states will push backwards into an old way of life, where the herd-immunity threshold is high. Dangerous decisions will be amplified by the dynamic systems of society. People will travel and seed outbreaks in places that have worked tirelessly to contain the virus. In some cases, a single infected person will indirectly lead to hundreds or thousands of deaths.
We have the wealth in this country to care for people, and to set the herd-immunity threshold where we choose. Parts of the world are illuminating a third way forward, something in between total lockdown and simply resuming the old ways of life. It happens through individual choices and collective actions, reimagining new ways of living, and having the state support and leadership to make those ways possible. For as much attention as we give to the virus, and to drugs and our immune systems, the variable in the system is us. There will only be as much chaos as we allow.
Related Podcast
Listen to James Hamblin discuss this story on an episode of Social Distance, The Atlantic’s guide to the pandemic:
Subscribe to Social Distance on Apple Podcasts or Spotify (How to Listen)
Via: The Atlantic